
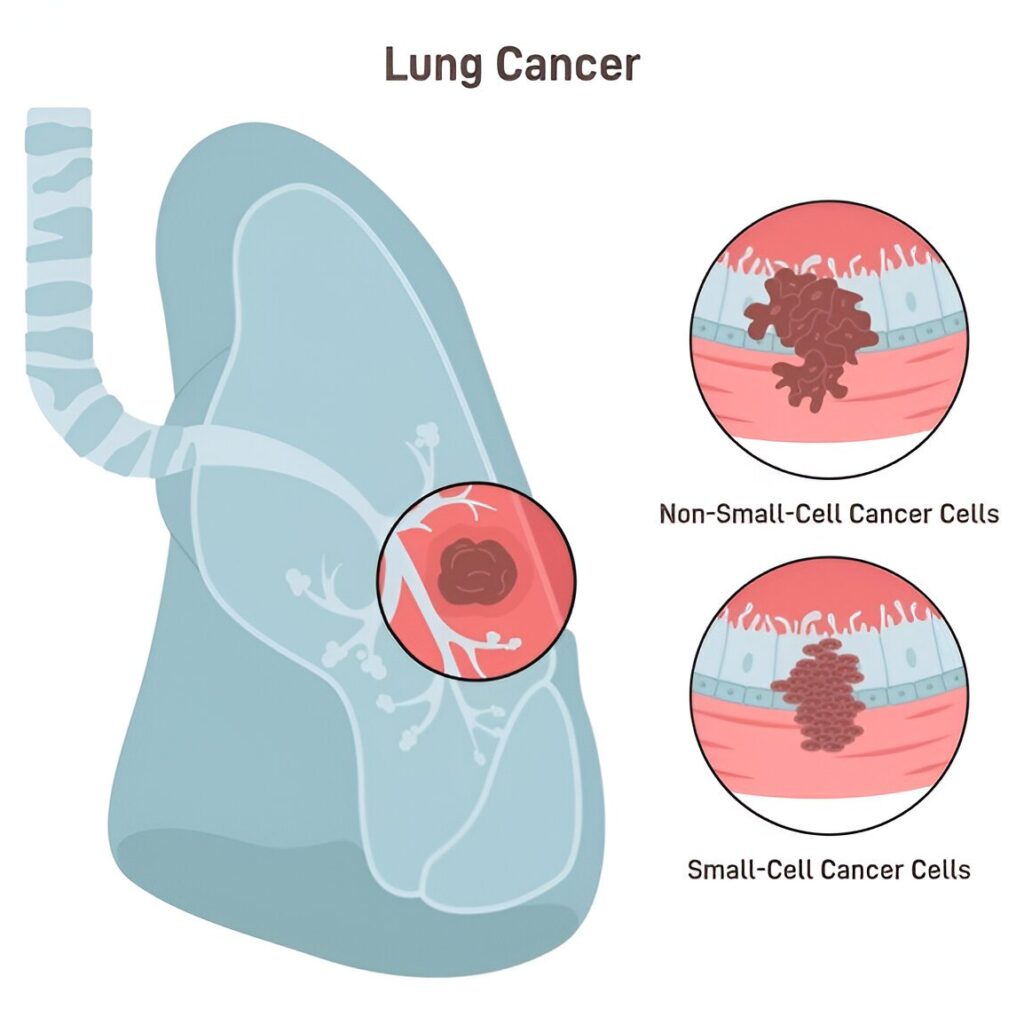
Non-small cell vs small cell lung cancer: Lung cancer is widely categorized into the following two major types: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). NSCLC constitutes an enormous majority of the disease cases,, between 80-85 percent and SCLC comprises about 10 to 15 percent. Such types vary in the appearance of cells, behavior, and therapy. The knowledge of these subtypes of lung cancer and their histology is paramount to making the appropriate choice of treatment.
NSCLC Overview: NSCLC itself has three main histologic subtypes:
- Adenocarcinoma: arises in outer lung areas from glandular (epithelial) cells.
- Squamous cell carcinoma: grows near the central airways (bronchi).
- Large cell carcinoma: can occur anywhere in the lung and tends to grow/spread faster than the other NSCLCs.
Each NSCLC subtype looks different under the microscope, but all are generally larger, glandular epithelial cells. By contrast, SCLC tumors are made of small, round cells (often called “oat cell” carcinoma) that look very tiny under a microscope. Importantly, SCLC is strongly linked to cigarette smoking – nearly all cases occur in smokers – whereas NSCLC can also appear in non-smokers (especially adenocarcinoma).
Key Differences: Non-small cell vs small cell lung cancer
- Prevalence: NSCLC is far more common (≈80–85% of lung cancers). SCLC is less common (~10–15%).
- Cell Size & Histology: NSCLC cells are larger and of varied types (adenocarcinoma, squamous, large cell). SCLC cells are small and densely packed, often described as “oat-like” under the microscope.
- Growth Rate: NSCLC tends to grow and spread more slowly. SCLC is highly aggressive – it grows quickly and often spreads (metastasizes) early.
- Smoking Link: Both types are linked to smoking, but SCLC is almost always caused by smoking, especially in heavy, long-term smokers.
- Symptoms and Spread: NSCLC symptoms may develop gradually (cough, weight loss, etc.) and tumors often stay localized longer. SCLC symptoms appear rapidly (sometimes with paraneoplastic syndromes) and SCLC frequently spreads to lymph nodes, brain, bones, liver and other organs.
- Subtypes and Histology: NSCLC subtypes (adeno, squamous, large-cell) are called “non-small cells” because their cells are bigger under histology. SCLC itself has two categories – “small cell carcinoma” and “combined small cell carcinoma” – based on cell appearance.
Overall, these differences mean NSCLC and SCLC are treated differently and have different prognoses.
Diagnosis and Histology: Non-small cell vs small cell lung cancer
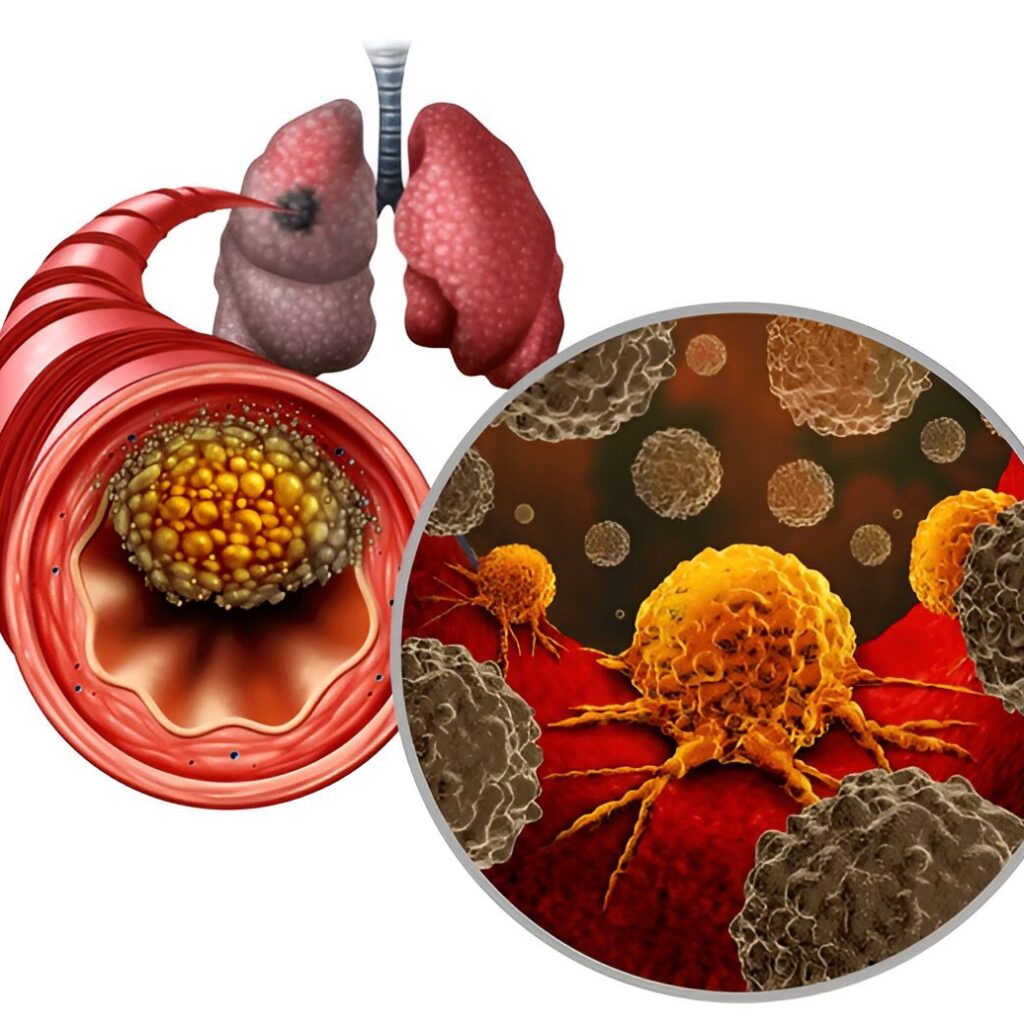
Lung cancer is diagnosed via imaging (X-ray, CT, PET) followed by biopsy. A pathologist examines tumor tissue under a microscope to identify the subtype. NSCLC and SCLC look very different histologically: as noted, NSCLC cells are larger and form distinct patterns (glandular or squamous layers), whereas SCLC cells are small, round, and often densely packed. Sometimes additional lab stains or molecular tests are done on the biopsy to confirm the diagnosis and look for gene changes (e.g. EGFR mutation) or proteins (like PD-L1). This “lung cancer profile” helps guide therapy choices.
Treating NSCLC: Multimodal Therapies
Treatment for NSCLC depends on stage (extent) and tumor subtype. Early-stage NSCLC (stages I–II) is often treated with surgery to remove the tumor. For example, only about 25% of NSCLC patients are diagnosed at stage I or II, and surgery (lobectomy or resection) is typically recommended in those cases. Surgery may be followed by adjuvant chemotherapy and/or radiation to lower recurrence risk. For stage III (locally advanced) NSCLC, a combination of chemotherapy and radiation (chemoradiation) is frequently used, sometimes followed by surgery.
In advanced NSCLC (stages IV), where cancer has spread, systemic therapies are key. In recent years, targeted therapies and immunotherapies have transformed NSCLC treatment. If tests find certain gene mutations (e.g. in EGFR, ALK, ROS1, KRAS, etc.), targeted drugs that attack those specific changes are used. For example, tumors with an EGFR mutation may be treated with osimertinib, while ALK-positive tumors use alectinib or similar inhibitors. Additionally, immune checkpoint inhibitors (immunotherapy) such as pembrolizumab, nivolumab, and others are now standard in NSCLC. These drugs target PD-1/PD-L1 pathways, unleashing the immune system on cancer cells. Blocking PD-1 “boosts the immune response against cancer cells,” helping to shrink tumors. Depending on PD-L1 levels and overall health, immunotherapy may be given alone or with chemo.
Summary of NSCLC therapies:
- Surgery: Main treatment for early-stage NSCLC.
- Chemotherapy: Used before/after surgery or for advanced disease.
- Radiation: Often combined with chemotherapy (especially in Stage III) or used if surgery isn’t possible.
- Targeted Therapy: For tumors with actionable mutations (EGFR, ALK, ROS1, MET, etc.).
- Immunotherapy: PD-1/PD-L1 inhibitors (e.g. pembrolizumab, nivolumab, atezolizumab, durvalumab) for advanced NSCLC.
Each patient’s treatment is tailored. For instance, a patient with Stage II NSCLC might have surgery followed by chemo, while a metastatic patient with an EGFR mutation would likely get a targeted drug. In all cases, multidisciplinary care (surgeons, oncologists, radiologists) is crucial.
Treating SCLC: Aggressive Combo Therapy
Because small cell lung cancer grows and spreads so quickly, its treatment is generally more aggressive and fast-paced. SCLC is divided into limited stages (confined to one hemithorax) and extensive stages (spread beyond) for planning treatment.
- Limited-stage SCLC: Standard treatment is chemotherapy plus concurrent chest radiation. Surgery is rarely used (only for very small solitary tumors that have not spread to lymph nodes). Chemotherapy usually uses etoposide plus a platinum drug (cisplatin or carboplatin). Concurrent radiation enhances cure chances, although it increases side effects. Because SCLC often metastasizes to the brain, prophylactic cranial irradiation (PCI) – low-dose brain radiation – is often given if the cancer responds well, to help prevent brain metastases.
- Extensive-stage SCLC: First-line therapy is chemotherapy plus immunotherapy. Typically, etoposide + platinum chemo is combined with a PD-L1 inhibitor (atezolizumab or durvalumab). This regimen can shrink tumors and is usually followed by immunotherapy maintenance. Unfortunately, even with treatment, almost all extensive-stage SCLC eventually relapses. Treatments focus on prolonging survival and alleviating symptoms.
Summary of SCLC therapies:
- Stage limited chemoradiation: Chemo + chest radiation.
- Chemotherapy: Core of treatment for all stages (etoposide + platinum).
- Immunotherapy (extensive stage): Add atezolizumab or durvalumab to chemo.
- Surgery: There is hardly any use; it is indicated only in rare cases of small tumors.
- Prophylactic Cranial Irradiation: This is usually administered in case of initial treatment failure.
Although SCLC is commonly responsive to chemo/radiation (and in most patients, it shrinks significantly), it is a rapidly relapsing tumor. First-line therapy results in remission in only a quarter of patients and will require subsequent treatment or clinical trials. Relapsed SCLC is examined with new drugs (such as lurbinectedin) and trials but the prognosis is difficult.
Prognosis and Outlook of Non-small cell vs small cell lung cancer
Generally, NSCLC has a better prognosis than SCLC, largely because it grows slower and often presents at an earlier stage. Early-stage NSCLC can sometimes be cured with surgery and adjuvant therapy. Five-year survival for localized NSCLC is much higher than for metastatic disease. SCLC, being aggressive, usually has worse overall survival – especially extensive-stage SCLC. However, immunotherapy and targeted drugs are improving outcomes in many cases.
In all cases, a detailed pathology report (lung cancer histology) and staging work-up guide expectations. For example, an NSCLC detected early as a small adenocarcinoma (stage I) might have a relatively favorable outlook after surgery, whereas an extensive-stage SCLC (with spread to brain or liver) requires systemic therapy and has a tougher prognosis. Talking with oncologists about stage and individual factors is important for understanding the outlook.
Conclusion and Key Takeaways
Non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC) are distinct diseases despite both arising in lung tissue. NSCLC is far more common, grows slower, and includes subtypes (adenocarcinoma, squamous, large cell). SCLC is rarer but far more aggressive, almost always linked to heavy smoking, and typically managed with urgent chemoradiation. Treatment advances – especially targeted therapy (for specific mutations) and immunotherapy – have improved care, particularly for NSCLC.
The selection of appropriate therapy requires the knowledge of the specific type and the stage of the cancer. This is the reason why pathology ( histology ) reports and staging tests are essential. When you have lung cancer (or a loved one), make sure to enquire about the type of subtype that is there, and the treatment that is most suitable. Early screening (e.g. through high-risk people getting low dose CT-scans on a regular basis) is another difference that can result in a significant difference since a lung cancer that is detected at an early stage is more treatable.
In general, the treatment of both NSCLC and SCLC needs to be done aggressively and with a customized treatment plan. Innovations keep on easing (immunotherapy, targeted drug, clinical trials), which brings about new hope. One should always be up to date with trusted channels and work hand in hand with oncologists in order to manage lung cancer care.
Call to Action
If you or someone you know is at risk for lung cancer (especially heavy smokers or former smokers), talk to a doctor about screening and early detection. Your oncology team needs to know about your pathology results and treatment options always. To learn more about lung cancer types and treatment, refer to such authoritative sources as the American Lung Association or Georgia cancer centers like Curepoint Cancer Center. Knowledge and action taken at an early stage can be critical.
Frequently Asked Questions
Q: What is the main difference between NSCLC and SCLC?
A: The key differences are cellular and behavioral. NSCLC cells are larger (non-small) and include adenocarcinoma, squamous, and large-cell types; it grows and spreads more slowly. SCLC cells are very small (oat-like) and the cancer is highly aggressive.
Q: Which type is more common?
A: Non-small cell lung cancer is much more common (about 80–85% of cases). Small cell lung cancer accounts for only 10–15% of lung cancers.
Q: How are treatments different?
A: NSCLC treatments often start with surgery (if caught early) and may include chemotherapy, radiation, targeted therapy (for gene mutations), and immunotherapy. SCLC treatment is usually chemotherapy combined with radiation right away; extensive SCLC also uses immunotherapy. Surgery plays a minor role in SCLC.
Q: What are lung cancer histology and subtypes?
A: “Histology” refers to how cancer cells look under a microscope. NSCLC has subtypes: adenocarcinoma (gland-like, peripheral lung), squamous cell (near airways), and large-cell (anywhere, fast-growing). SCLC histology shows tiny round cells (“small cell carcinoma”). These distinctions guide treatment choices.
Q: Can targeted or immunotherapy help in SCLC?
A: Recently, PD-L1 immunotherapy drugs (atezolizumab, durvalumab) have been approved for extensive-stage SCLC when added to chemotherapy. Targeted therapies (EGFR/ALK drugs) are generally specific to NSCLC subtypes with those mutations, so they’re not used in classic SCLC.
Q: How important is smoking cessation?
A: Very important. The primary cause of both NSCLC and more so SCLC is smoking which not only lowers your risk of getting lung cancer it also enhances treatment response and survival in case you have lung cancer.


Add a Comment