Prostate cancer is one of the most commonly diagnosed cancers in men, especially among those over the age of 50. With early detection and timely medical care, prostate cancer is highly treatable. Access to advanced healthcare facilities and experienced specialists plays a critical role in improving survival rates and quality of life. This blog provides a detailed overview of prostate cancer treatment in Georgia, while also highlighting how global medical expertise, including options in Dublin, can support comprehensive cancer care through Cure Point Cancer.
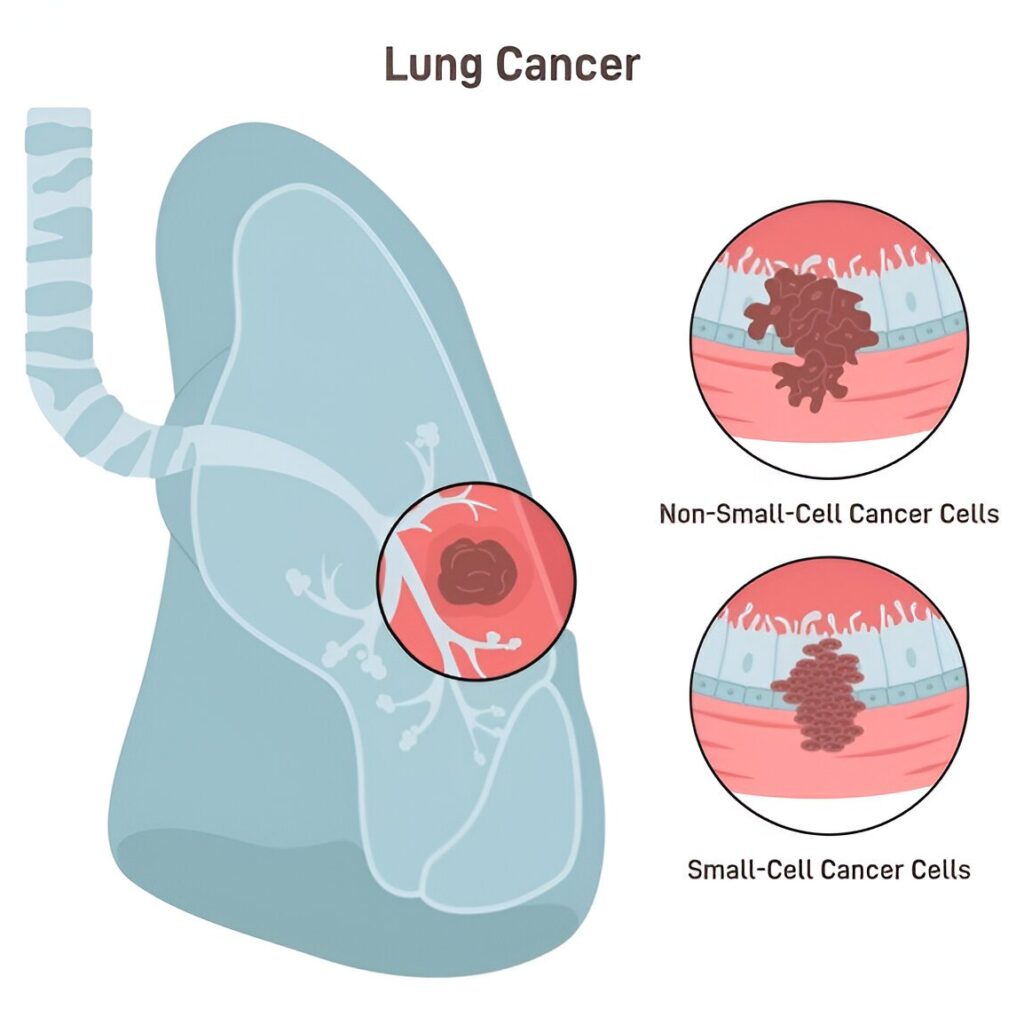
Understanding Prostate Cancer
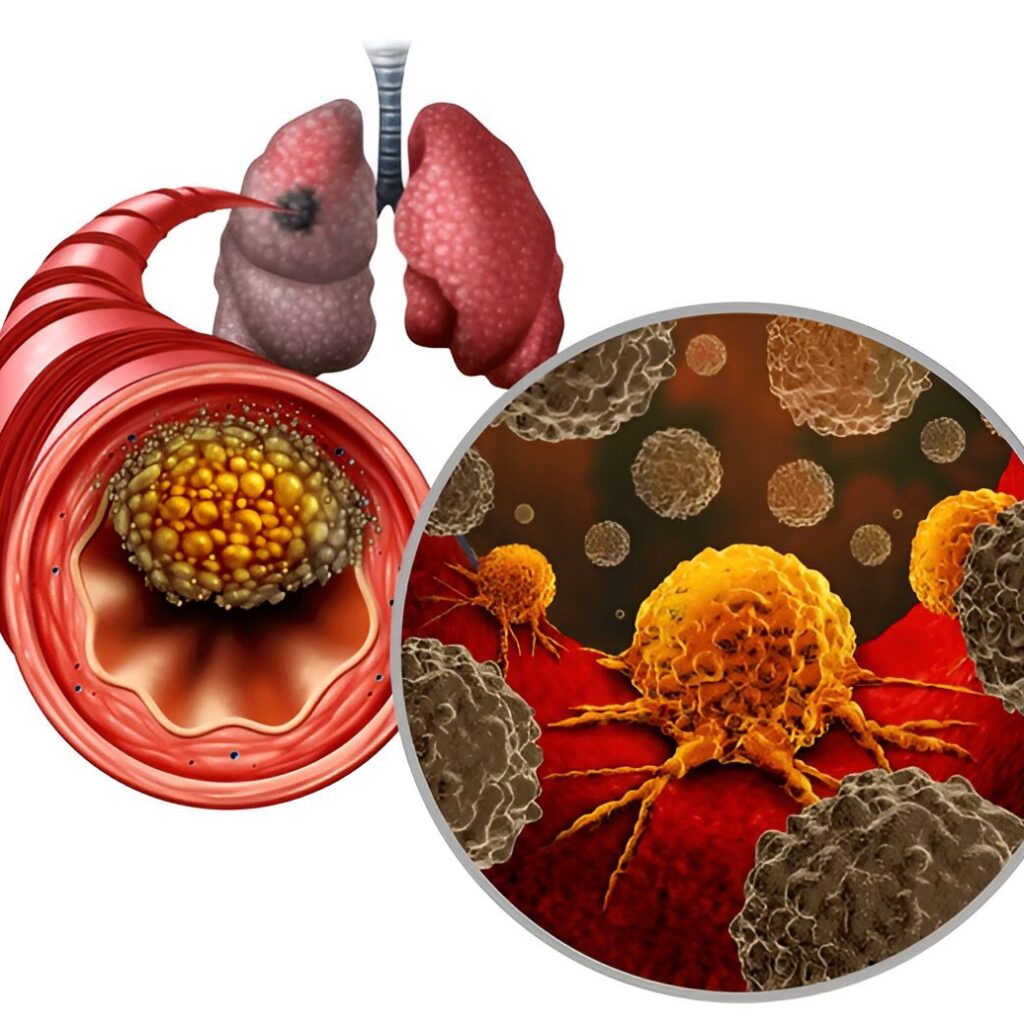
Prostate cancer develops in the prostate gland, which is responsible for producing fluid that nourishes and transports sperm. In many cases, prostate cancer grows slowly and may not cause immediate symptoms. However, aggressive forms can spread rapidly and require prompt treatment.
Common risk factors include:
- Increasing age
- Family history of prostate cancer
- Genetic factors
- Lifestyle and dietary habits
Because early-stage prostate cancer often shows no symptoms, regular screening is essential for early diagnosis.
Prostate Cancer Treatment in Georgia: An Overview
Prostate cancer treatment in Georgia has advanced significantly over the years. The state is home to modern cancer centers offering comprehensive diagnostic services, cutting-edge treatment technologies, and multidisciplinary care teams. Patients in Georgia benefit from access to:
- Advanced imaging and diagnostic tools
- Highly trained urologists and oncologists
- Minimally invasive surgical options
- Precision radiation therapy
- Personalized treatment planning
Georgia’s healthcare ecosystem focuses on evidence-based treatment protocols and patient-centered care, making it a preferred destination for prostate cancer management.
Importance of Early Detection
Early detection is one of the most important factors in successful prostate cancer treatment in Georgia. Routine screening allows doctors to identify cancer before it spreads beyond the prostate.
Key screening methods include:
- PSA (Prostate-Specific Antigen) blood test
- Digital Rectal Examination (DRE)
- MRI for high-risk or abnormal PSA cases
When prostate cancer is diagnosed at an early stage, treatment options are more effective and less invasive.
Diagnosis and Staging
Accurate diagnosis and staging are essential before starting prostate cancer treatment in Georgia. This process may involve:
- Prostate biopsy to confirm cancer
- Gleason score to assess cancer aggressiveness
- Imaging tests such as MRI, CT scans, or bone scans to determine cancer spread
These diagnostic steps help doctors create a tailored treatment plan based on the patient’s specific condition.
Treatment Options for Prostate Cancer in Georgia
Prostate cancer treatment in Georgia is highly personalized and depends on cancer stage, age, overall health, and patient preferences. The main treatment options include:
1. Active Surveillance
For low-risk and early-stage prostate cancer, active surveillance may be recommended. This approach involves:
- Regular PSA testing
- Periodic imaging
- Repeat biopsies if needed
Active surveillance allows patients to avoid or delay treatment side effects while closely monitoring disease progression.
2. Surgery (Radical Prostatectomy)
Surgery is one of the most common methods of prostate cancer treatment in Georgia, especially for localized cancer. The prostate gland is surgically removed to eliminate cancer cells.
Advanced surgical techniques available in Georgia include:
- Minimally invasive laparoscopic surgery
- Robotic-assisted prostatectomy
These methods often result in faster recovery times, reduced pain, and improved outcomes.
3. Radiation Therapy
Radiation therapy uses high-energy beams to destroy cancer cells and is a key option in prostate cancer treatment in Georgia. It may be used as a primary treatment or after surgery.
Types of radiation therapy include:
- External Beam Radiation Therapy (EBRT)
- Brachytherapy (internal radiation)
Modern radiation techniques improve precision and reduce damage to surrounding healthy tissue.
4. Hormone Therapy (Androgen Deprivation Therapy)
Hormone therapy lowers testosterone levels, which helps slow the growth of prostate cancer cells. It is commonly used in advanced or recurrent prostate cancer cases.
Hormone therapy may be combined with radiation or other treatments for better outcomes.
5. Chemotherapy and Targeted Therapy
For advanced or metastatic prostate cancer, chemotherapy may be recommended. Targeted therapies focus on specific genetic or molecular features of cancer cells, improving effectiveness while minimizing side effects.
Georgia’s cancer centers offer access to these advanced systemic treatments under expert supervision.
6. Immunotherapy
Immunotherapy is an emerging option in prostate cancer treatment in Georgia for select patients. It works by stimulating the body’s immune system to recognize and fight cancer cells. While not suitable for all cases, it offers promising results in advanced disease.
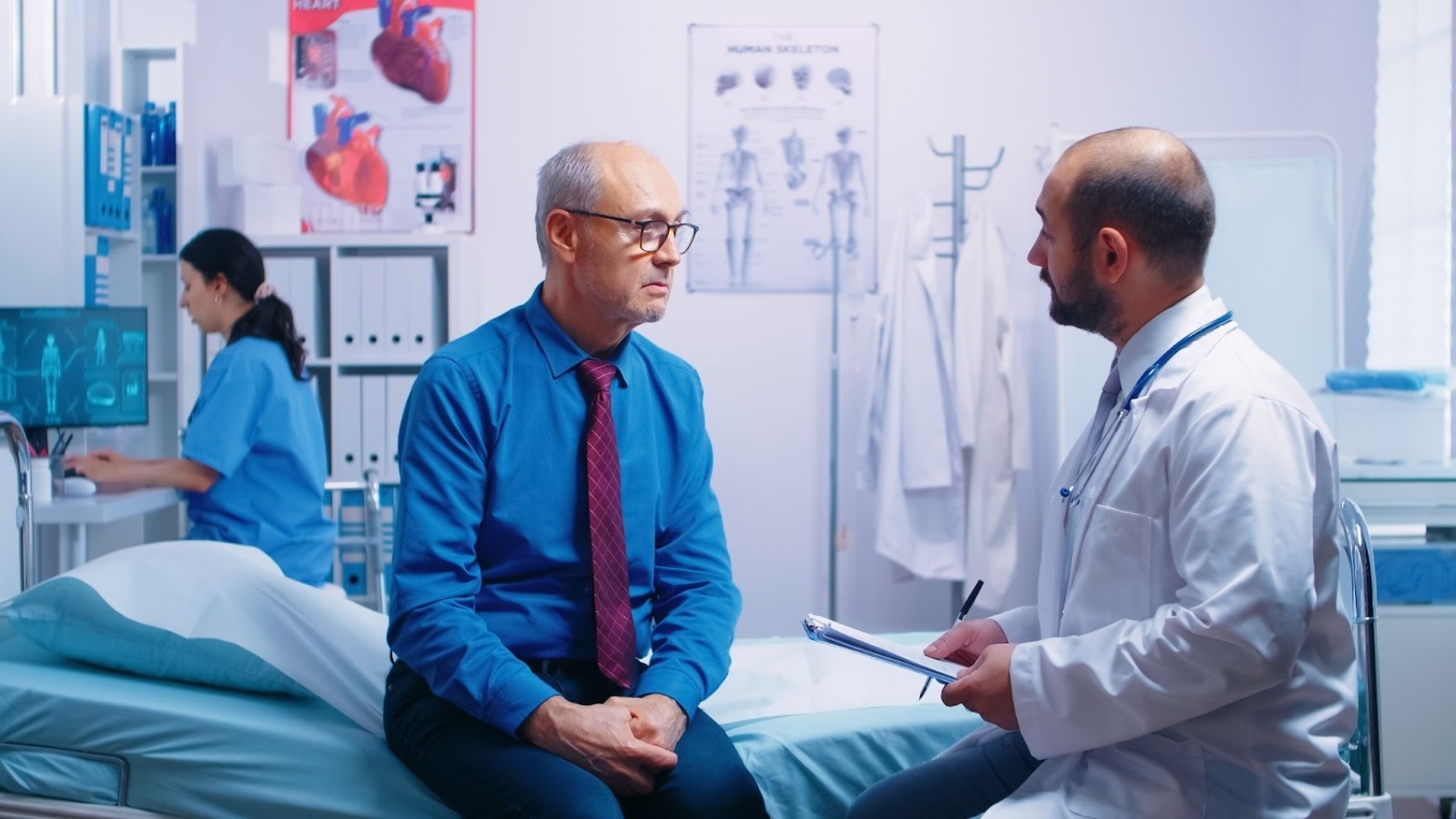
Multidisciplinary Cancer Care Approach
A key strength of prostate cancer treatment in Georgia is the multidisciplinary care model. Treatment teams typically include:
- Urologists
- Medical oncologists
- Radiation oncologists
- Radiologists
- Pathologists
- Oncology nurses
This collaborative approach ensures comprehensive evaluation, coordinated treatment planning, and continuous patient support.
At Cure Point Cancer, multidisciplinary collaboration is central to delivering high-quality prostate cancer care.
Role of Dublin in Advanced Prostate Cancer Care
While Georgia remains the primary focus for treatment, Dublin serves as an important global medical hub for advanced oncology care and research. Some patients may explore international expertise, clinical trials, or second opinions from Dublin-based specialists through coordinated care pathways.
Cure Point Cancer helps patients navigate global treatment insights while ensuring continuity of care within Georgia whenever required.
Supportive Care and Quality of Life
Effective prostate cancer treatment in Georgia goes beyond medical therapy. Supportive care services play a crucial role in maintaining quality of life, including:
- Management of urinary and sexual health side effects
- Psychological counseling and emotional support
- Pain management and rehabilitation
- Lifestyle and nutrition guidance
These services help patients and families cope with the physical and emotional challenges of prostate cancer.
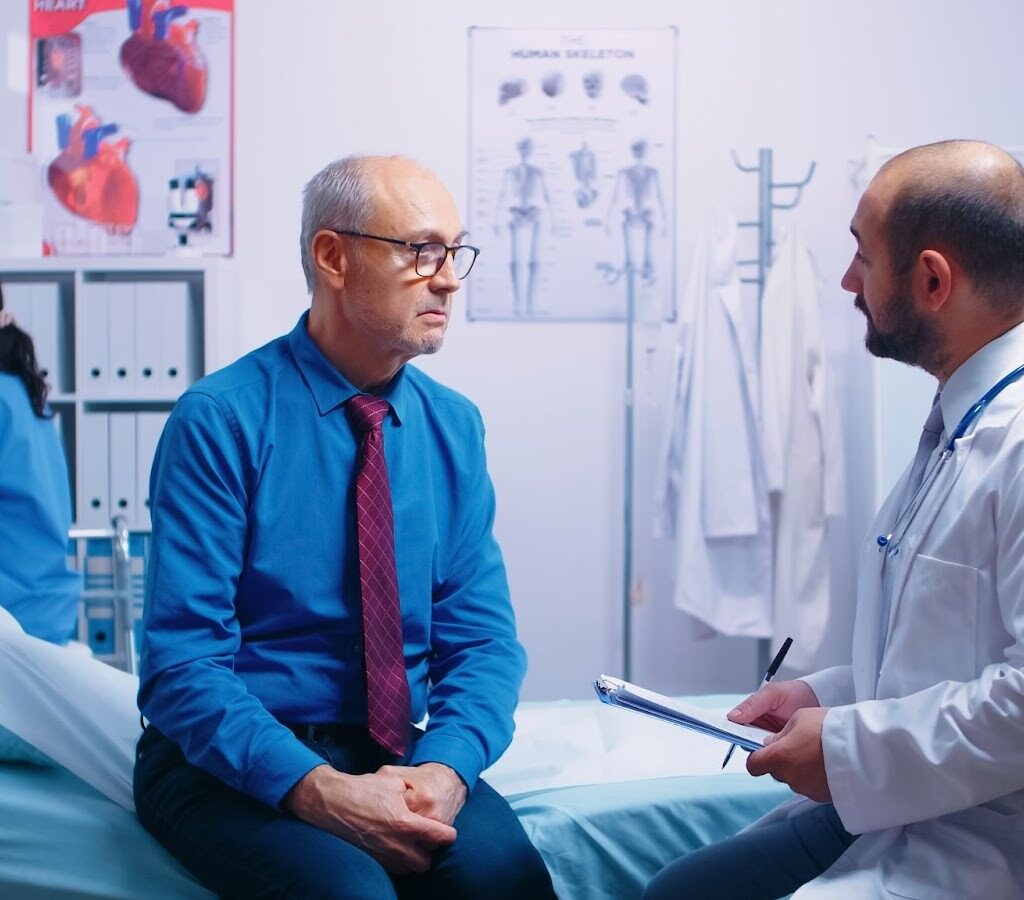
Why Choose Cure Point Cancer for Prostate Cancer Treatment in Georgia?
Cure Point Cancer is committed to delivering personalized, advanced, and compassionate prostate cancer care. Patients choose Cure Point Cancer for:
Individualized Treatment Plans
Each patient receives a customized approach based on cancer stage, health condition, and personal preferences.
Advanced Medical Technology
Access to modern diagnostic tools, precision surgery, radiation therapy, and systemic treatments.
Experienced Oncology Specialists
Highly skilled teams with expertise in prostate cancer management.
Patient-Centered Support
From diagnosis to recovery, Cure Point Cancer prioritizes patient education, comfort, and long-term well-being.
Life After Prostate Cancer Treatment
Life after prostate cancer treatment in Georgia involves regular follow-ups, PSA monitoring, and long-term health management. Survivorship care focuses on:
- Monitoring for recurrence
- Managing treatment side effects
- Promoting healthy lifestyle changes
- Emotional and mental well-being
Many patients go on to live healthy, active lives after successful treatment.
Conclusion
Prostate cancer treatment in Georgia offers patients access to advanced medical care, experienced specialists, and comprehensive support systems. Early detection, accurate diagnosis, and personalized treatment planning are key to successful outcomes. With expert guidance from Cure Point Cancer, patients can confidently navigate their treatment journey while benefiting from both local excellence and global medical insights.
If you or a loved one is seeking trusted prostate cancer treatment in Georgia, Cure Point Cancer is here to provide expert care, compassion, and hope at every step.